Supporting elderly and vulnerable patients
There are real fears around what the wider effects of the pandemic on the most vulnerable patients. In the early part of March, the Hillview Nursing Team suggested an initiative to offer ‘wellbeing health checks’ to vulnerable patients. These range from organising electronic prescriptions to general discussions about health, such as mental health and their ability to cope with daily activities.
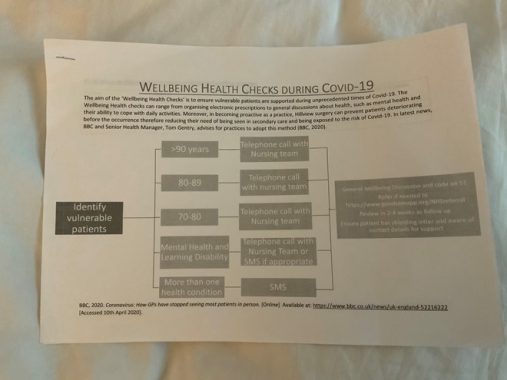
The project commenced in March 2020 with a search run on System One to identify vulnerable patients and categorised into groups as follows: >90 years, 80-89 years, 70-80 years, mental health and learning disability and more than one health condition. A spreadsheet was created to record the details. The plan was for the nursing team to ring these patients systematically as per the workflow template (Appendix A).
The content of the telephone consultations by the nursing team included general wellbeing discussions, ensuring patients have received the shielding letter, contact details for support available for such patients and the choice of referring such patients to GoodSAM, the voluntary NHS support service. The idea was for the nursing team to either encourage patients to self-refer or refer on behalf of the patients.
GoodSAM offers support to high risk vulnerable patients who have been advised to self-isolate. The services offered include as follows:
- Check in and Chat Support: Provides short-term telephone support to individuals who are at risk of loneliness as a consequence of self-isolation.
- Community Support: Provides collection of shopping, medication or other essential supplies for someone who is self-isolating, and delivering these supplies to their home.
- Patient Transport Support: Provides transport for patients who are medically fit for discharge or to support patients going to NHS appointments.
- NHS Transport Support: Provides transport for equipment, supplies and/or medication between NHS services and sites. Also involves assisting pharmacies with medication delivery.
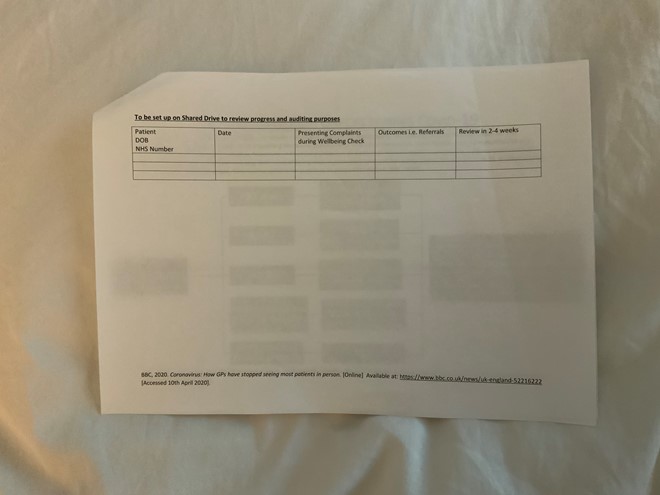
‘Review call’ was set up by the nurses and patients were followed up every two to four weeks. In addition, the team completed the consultations by entering a code on System One (‘well being visit’ and ‘referral to NHS volunteers’). A spreadsheet (see pic) was set on Shared Drive to review progress and future auditing purposes. Patients with ongoing issues lasting four weeks were referred to our social prescriber.
The initial verbal feedback from patients after four weeks was that many were not aware of the voluntary services, were thrilled to become part of this service offered. Patients welcomed the idea as many were lonely and felt they were recognised/not forgotten and valued in the community. The calls were carried out during the early part of the response to the pandemic, despite the Hillview team being extremely busy responding to the pandemic.
Those most vulnerable were able to get the help they needed with shopping and getting their medications delivered, as well as increasing awareness of the services available to them. In addition, the nursing team also took the opportunity to update their next of kin in their record for onward planning of their care. The team also addressed their physical needs in addition to their social aspect of care, providing home visits for blood tests and BP checks.
This project was worthwhile and satisfactory. Our elderly vulnerable patients felt grateful that they were continuously looked after during these hard times.
Our staff have signed up to continue to offer similar service even if the current voluntary GoodSAM service will no longer be available beyond the Covid -19 pandemic. The idea is to look into all such voluntary services available to patients and formulate an information sheet to share with patients during our ‘wellbeing healthchecks’.
Hillview team also signed up to continue and extend such ‘wellbeing health checks’ service to all patients with chronic long-term conditions. The intention is to manage the majority of such patients via telephone and/or video consultations as part of the review of long-term medical management. In addition, Hillview plans to have our HCA follow up such patients routinely via telephone, by allocating such patients to a weekly wellbeing healthchecks clinic. There are ongoing discussions to extend this role to our administrative team with a view to becoming a ‘health and wellbeing coordinator’, ‘health coach’ or similar role.
Ongoing plan
The next step is to obtain feedback via a Hillview staff and Patient survey on the service (within 6-12 months), collating feedback on suggested improvements, to assess if the service offered is sustainable and further document the benefits for our patients.
The intention is to collate all the feedback and to share with our PPG members. In addition, we plan to discuss the outcome in our clinical, practice and staff meetings; any suggested improvements will be discussed collectively and agree on the one or two areas of improvement that will be taken forward to implement. If successful, we plan to revisit the feedback by patients biannually.
Source: Information shared with Pulse by Dr Vasu Siva,GP partner at Hillview Surgery, west London [provided 14 May]
